A group of musicians, all suffering, to varying degrees, from dementia, Alzheimer’s or Parkinson’s disease, call themselves The Fifth Dementia and jam together twice a week. PBS NewsHour visited with the musicians and their families to learn how music has made a difference in their lives, by helping them stay active and connected. You can read the report and watch a video here.
Neuroscience Public Lecture: “Degeneration in the Aging Brain,” March 12
The students of the Penn Neuroscience Graduate Group are hosting a Neuroscience Public Lecture entitled “Degeneration in the Aging Brain,” on Thursday, March 12th in Smilow Auditorium at 6:30pm. This FREE event will feature 3 fifteen minute TED-style talks from Penn Neuroscience faculty Virginia Lee, Alice Chen-Plotkin, and Harry Ischiropoulos. A reception will follow.
Registration and more information can be found here (https://nggglia.wordpress.com/neurolecture/).
Date: Thursday, March 12th, 6:30pm (Check-in begins at 6pm)
Location: Smilow Center for Translational Research Auditorium, 3400 Civic Center Blvd, Philadelphia, PA, 19104
Silicon Valley Start Up Hopes to Catch Alzheimer’s Before Memory Slips
A Silicon Valley health start-up, Neurotrack, is developing a computerized visual test that aims to accurately identify people at risk of Alzheimer’s. The test requires no language or motor skills; participants view images on a monitor while a camera tracks their eye movements. According to Scientific American, “The test draws on the research of Neurotrack co-founder Stuart Zola of Emory University who studies learning and memory in monkeys. When presented with two images—one novel, the other familiar—primates will fixate longer on the novel one. If the hippocampus is damaged, as it is in Alzheimer’s, however, the subject spends equal time looking at each image.”
You can read the Scientific American article here.
Submit Your Posters Now for the May 5, 2015 IOA Retreat
Registration is open for the IOA’s May 5 Sylvan M. Cohen 2015 Annual Retreat: “Aging with Financial Security: Addressing the Challenges of Cognitive Aging and Impairment.” Poster submission is now open as well. Click here to submit your poster information. Deadline for poster submission is April 24.
A fear of the future: Researchers find that the prospect of decline – not the label of “Alzheimer’s disease”- drives negative feelings about a person with dementia
A study has uncovered what causes people to experience stigmatizing reactions to persons with Alzheimer’s disease dementia.
Researchers –including Rebecca Johnson, M.A. Princeton University Department of Sociology, Jason Karlawish, MD, associate director of the Penn Memory Center, Pamela Sankar, PhD of the Department of Medical Ethics and Health Policy, and Kristin Harkins, research coordinator at the Penn Memory Center — presented these results at the American Public Health Association annual meeting in November 2014.
“This project on Alzheimer’s stigma was sparked by an observation,” says Johnson. “Although researchers, clinicians and the public often talk about how those with Alzheimer’s face stigma, there was a lack of clarity about what features of Alzheimer’s prompt stigmatizing reactions in others.”
The online experiment with 800 adults from the U.S. general population had participants read a story about a patient with symptoms that described mild stage dementia. Participants were randomized to one of nine unique stories that differed in two key features: the disease label (“Alzheimer’s” versus “traumatic brain injury” versus no label), and the prognosis (“symptoms will get better” versus “stay the same” versus “worsen”). Next, the participants answered questions about their attitudes towards the person in the story, such as what emotions they felt and whether they thought the patient’s friends would start to distance themselves from the patient.
All participants read a story about a man with mild stage dementia, but some read that his disabilities were caused by Alzheimer’s while others read that that they were caused by brain injury or they did not have a cause. And the prognosis varied as well. These variations in the label and the prognosis allowed the researchers to test whether the disease label or the prognosis drive stigmatizing reactions.
Learning that the dementia symptoms were caused by Alzheimer’s didn’t prompt more stigmatizing responses than from the other possible causes. In short, the disease label did not influence stigma. Instead, stigmatizing reactions were more likely from people whose story described that the patient’s symptoms would get worse.
The study suggests that one of the best ways to minimize stigmatizing reactions for Alzheimer’s patients is to emphasize the range of clinical outcomes and prognoses people may have. The researchers concluded that it is also important that public messaging around Alzheimer’s should reflect the broad range of levels of the disease rather than just the most severe cases. Most importantly, the results suggest the need to understand the potential for stigma in persons in the “pre-clinical” stage of the disease. This stage — which is still under study and not yet used in clinical practice — describes an asymptomatic person who has Alzheimer’s biomarker pathology. It is a stage defined by prognosis and if this study of stigma is correct, then people with the label may experience stigma.
To listen to a recording of the presentation at the APHA meeting, click here.
In Alzheimer’s Cases, Financial Ruin and Abuse Are Always Lurking
In a Wealth Matters column in The New York Times, stories from financial advisers illuminate the challenges for patients and their families. You can read the column here.
Watch the Alzheimer’s Research Summit on February 9 and 10
Watch the Alzheimer’s Research Summit live on Feb 9 and 10 at http://videocast.nih.gov/ and follow on Twitter @ADSummit15 for highlights.
PMC is Moving to the Penn Neuroscience Center
On February, 23, 2015, the Penn Memory Center at the Perelman Center for Advanced Medicine will be moving down the hall to the new Penn Neuroscience Center.
Our address remains the same:
Penn Memory Center at the Penn Neuroscience Center
Perelman Center for Advanced Medicine
3400 Civic Center Boulevard, South Pavilion, 2nd Floor
Philadelphia, PA 19104
Save the Date! Institute on Aging’s Sylvan M. Cohen 2015 Annual Retreat
Join us on May 5, 11:30am – 5:00pm, for the Institute on Aging’s Sylvan M. Cohen 2015 Annual Retreat: “Aging with Financial Security: Addressing the Challenges of Cognitive Aging and Impairment.”
A rapidly aging U.S. population means older adults’ financial well-being and security is becoming an urgent public health concern. The five million people living with Alzheimer’s disease dementia are vulnerable to financial abuse or exploitation, or bad financial decisions. In addition, age-related cognitive changes also put older adults at risk. These problems are especially significant as older adults may have limited time or capacity to recover financial losses. “Aging with Financial Security: Addressing the Challenges of Cognitive Aging and Impairment” will examine the nature and scope of the problem, its challenges, and possible solutions. Experts in adult protective service, academics, advocacy and government will present cutting edge research and innovative solutions to support the financial well-being of older adults.
For more information email Aging@mail.med.upenn.edu or call 215-898-7801.
The deadline to participate in the poster session is April 24, 2015.
Art for Alzheimer’s
Philly Voice recently published a feature about ARTZ Philadelphia’s program to connect dementia patients with art, and its partnership with the Penn Memory Center. Felicia Greenfield, associate director for clinical and research operations at the Penn Memory Center, was interviewed for the article about funding issues in Alzheimer’s research and care.
To read the article, click here.
Complexities of Choosing End-of-Life Strategies for Those with Dementia
A New York Times article looks at the debate about whether people who develop dementia can use “voluntarily stopping eating and drinking” (VSED ) or other strategies to end their lives by including such instructions in an advance directive.
Dementia rates and numbers have begun a steep ascent, already afflicting an estimated 30 percent of those older than 85. Baby boomers are receiving a firsthand view of the disease’s devastation and burdens as they care for aging parents.
To read the article, click here.
Philadelphia Inquirer Features PMC’s A4 Study
Philadelphia Inquirer reporter Stacey Burling interviewed Penn Memory Center research participants and clinicians in her article about the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s (A4) Study, entitled “The risk of knowing: Alzheimer’s research volunteers.“
The A4 Study is a historic clinical trial to see if an experimental drug can protect healthy seniors whose brains harbor silent signs that they’re at risk. Ms. Burling spoke with Myrna Roach and Donald Jackson about why they chose to enroll in the study. She also spoke with Jason Karlawish, MD, associate director of the PMC about his A4 sub study which measures how disclosure of study participants’ amyloid status impacts them.
You can read the article here.
Interested in enrolling in the A4 study? Click here for more information.
Penn Memory Center Launches Brain Health Research Registry
The Penn Memory Center has launched a new Brain Health Research Registry. By enrolling in the Penn Memory Center’s Brain Health Research Registry you can play a vital role in research. The Registry serves as the research recruitment resource for investigators at the Penn Memory Center who are studying brain diseases such as Alzheimer’s disease, which affects over 5 million people in the US.
The Penn Memory Center Brain Health Research Registry is a confidential database that is made up of people like you who have volunteered to consider participation in research studies. We will contact you periodically with a list of research studies that you may consider joining. Participation is always optional and all information is kept confidential.
For more information, please contact Tigist Hailu, Coordinator for Diversity in Research, at tigist.hailu@uphs.upenn.edu or 215-573-6095. You can download a Brain Health Research Registry card here.
Philadelphia Tribune Features Penn Memory Center
A recent Philadelphia Tribune article highlights Penn Memory Center and their work towards raising awareness of Alzheimer’s Disease in the African American community. You can read the article here.
Writing the Medical Narrative
Writer Deborah Fries, a contributor to Penn Memory Center’s InSight newsletter and the makingsenseofalzheimers.org website, is teaching an online class, “Writing the Medical Narrative,” this winter through the Loft Literary Center.
“Medical narratives are often passports to otherness, transporting us deep into the far country of an illness,” Ms. Fries says. “And like all good travel writing, they rely heavily on description to delineate a foreign terrain or to resonate with those who have already traveled there.”
“To understand the otherness of an illness or the unseen microscopic works of the body,” she adds, “writers rely on figurative language. The poetic metaphors, similes, and practical analogies that we make give our writing its tone, its heft—and most of all, its agency to affect the reader.”
To learn more about the class, visit the Loft Literary Center.
Alzheimer’s Accountability Act Incorporated into Funding Bill Signed into Law
Congress has created a formal process to ensure that scientific judgment will guide them in future Alzheimer’s research funding. The Alzheimer’s Accountability Act, which was fully incorporated within the fiscal year 2015 funding bill signed into law by the President on December 17, 2014, ensures that funding levels determined by Congress are based on scientific recommendations of the National Institutes of Health. Funding for Alzheimer’s research was also increased by $25 million through this bill.
For more information, click here.
Dr. Martin Luther King, Jr. Health Equity Symposium
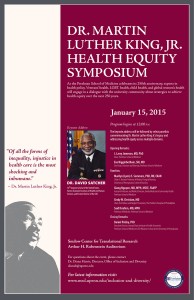 Please join the university community in commemorating Dr. Martin Luther King Jr.’s legacy on January 15, 2015 at noon in the Arthur H. Rubenstein Auditorium at the Smilow Center for Translational Research. This is the first in a series of talks celebrating the Perelman School of Medicine’s 250th anniversary that will address disparities through dialogue, with the goal of achieving health equity for all in the next 250 years.
Please join the university community in commemorating Dr. Martin Luther King Jr.’s legacy on January 15, 2015 at noon in the Arthur H. Rubenstein Auditorium at the Smilow Center for Translational Research. This is the first in a series of talks celebrating the Perelman School of Medicine’s 250th anniversary that will address disparities through dialogue, with the goal of achieving health equity for all in the next 250 years.
“Of all the forms of inequality, injustice in health care is the most shocking and inhumane.” -Dr. Martin Luther King, Jr.
For more information, click here.
Jason Karlawish, MD Visits Studios of “Second Opinion” for Television Taping
Jason Karlawish, MD, Associate Director of the Penn Memory Center visited the Rochester, NY studios of Second Opinion for an in-depth discussion about one woman’s experience with her mother’ s decline into Alzheimer’s disease, and the signs that were missed or symptoms that were ignored.
The current standard of care or those with Alzheimer’s disease, Dr. Karlawish says, is “education and counseling of the patient and family; symptomatic treatment of the disease and longitudinal follow-up at least every six months to assess rate of progression.”
Second Opinion airs on public television stations through the country. You can view the episode here.
Alzheimer’s is Greater Public Health Crisis than Ebola
David Satcher, MD, former director of the CDC and former Surgeon General, writes in The Hill, “Our nation is facing a far more dangerous public health crisis than Ebola, and the response has been altogether inadequate.”
“While Ebola is a potential disaster in the United States we must address decisively, Alzheimer’s disease is already today a deadly disaster for millions of American families that we have largely ignored. It is a threat to both public health and to our economy. That is what should frighten people,” he adds.
To read the full article, please click here.
How Old is Too Old? Two Ethicists Debate Quality of Life as We Age
What happens when you bring two medical ethicists together to discuss what it means to age with quality of life? A fascinating debate ensues. On WHYY FM recently, two medical ethicists discussed and debated what quality of life means as we age. You can listen to Jason Karlawish, MD, Associate Director of the Penn Memory Center, and Zeke Emanuel, chair of the Department of Medical Ethics and Health Policy at the University of Pennsylvania, on WHYY”S The Pulse.
What’s Good For Your Heart is Good For Your Brain
On Saturday, November 22, 2014, over 150 people from the Philadelphia community joined Penn Memory Center and First Corinthian Baptist Church in West Philadelphia for their Cognitive Health Fair.
The fair, which was a collaborative effort between the Center (PMC) and one of their research participants and Community Advisory Board members, Ms. Elsie Shelton, targeted local seniors to educate them on the importance of blending a healthy diet, physical exercise, and social and mental engagement to maintain both cognitive and heart health. After all, what’s good for your heart is good for your brain.
The day kicked off with words of appreciation from Pastor Thomas of First Corinthian Baptist Church and Dr. Jason Karlawish, Associate Director of the Penn Memory Center. The fair provided a variety of services to the community including:
- free glaucoma screenings from the Scheie Eye Institute
- blood pressure screenings and health education materials from Penn Geriatric’s Nurse Practitioner Johanne Louis
- giveaways and education materials provided by Penn Dental students
- healthy brain aging handouts and research opportunities from Penn Memory Center
- caregiver support resources from Jean Kirkley of Boomer R Heroes
- educational materials about AD and caregiver support from Rev. Barbara Jones of the Delaware Valley Chapter of the Alzheimer’s Association
- information about the Philadelphia Games which is an Olympic style event for people 50 years of age and older distributed by the City’s Parks and Recreation
For more information please contact Tigist Hailu at tigist.hailu@uphs.upenn.edu .
What To Do if You Notice a Loved One “Slipping Away” This Holiday Season
In a recent Today Health article, Penn Memory Center’s Jason Karlawish, MD shares his insight on what to do if you notice a loved one “slipping away” this holiday season.
“The classic story I see is when the holidays come and the older adult doesn’t do the things they traditionally have,” says Dr. Karlawish. “For example, dad always did his special pecan pies, and when Thanksgiving comes there are no pies or they are a disaster. For many, those may be the first symptoms that show that a parent can’t do everyday tasks anymore.” You can read the article here.
2014 Thank You Breakfast
Saturday, November 8, 2014, was a day to honor Penn Memory Center research participants and their study partners. More than 200 people attended the 8th annual Penn Memory Center Thank You Breakfast at the Inn at Penn.
With the theme of “Without research there can be no progress against Alzheimer’s disease or better understanding of healthy brain aging …and without you, there can be no research,” the annual invitation-only breakfast thanks research participants for their contribution to Penn’s Alzheimer’s disease research.
John Trojanowski, MD, PhD, director of Penn’s Alzheimer’s Disease Core Center; Steven E. Arnold, MD, director of the Penn Memory Center; Jason Karlawish, MD, associate director of the Penn Memory Center; David Wolk, MD, assistant director of the Penn Memory Center; Felicia Greenfield, LCSW, associate director for clinical and research operations at the Penn Memory Center; Marianne Watson, RN, PMC’s senior research nurse, and Tigist Hailu,PMC’s coordinator for diversity in research, presented the latest results from their research studies as well as updates on Penn Memory Center programs and upcoming research opportunities.
Balancing Old Age with Happiness
Kathleen Dunn of Wisconsin Public Radio interviewed Jason Karlawish, MD, Associate Director of the Penn Memory Center, to discuss his belief that as we age we desire not simply to pursue life, but happiness, and that medicine is important, but it’s not the only means to this happiness. You can listen to the interview here.
University of Pennsylvania Institute on Aging and Alzheimer’s Disease Core Center Pilot Study Announcement
The University of Pennsylvania Institute on Aging (IOA) and Alzheimer’s Disease Core Center (ADCC) will fund up to six (6) one-year multidisciplinary pilot grants in the 2015-2016 academic year to support biomedical, epidemiological, behavioral or health services research, as well as basic science, clinical or psychosocial research. Two of the pilots, funded by Penn’s ADCC, will focus on Alzheimer’s disease (AD) and related neurodegenerative disorders as well as healthy brain aging. The remaining pilots, supported by funding from the Perelman School of Medicine at Penn (PSOM) to the IOA, will focus on aging and aging-related diseases as well as healthy aging.
Applicants may consider using data from the National Alzheimer’s Coordinating Center. More information can be found at their website: https://www.alz.washington.edu/.
The Principal Investigator (PI) for each of these pilots must be a member of the University of Pennsylvania fulltime faculty from any of its 12 schools. Collaboration with other departments or schools is strongly encouraged. In addition, applicants who want to be considered for the Penn ADCC pilots must ensure that the PI for the pilot commits some effort to the project.
Each pilot will be funded at a level of up to $50,000/year for personnel and supply costs, but not tuition costs, student dissertation research, equipment or instruments. The purpose of these one-year, non-renewable grants is to assist faculty in obtaining preliminary data to serve as the basis of a grant application to the NIH or other public or private agencies concerned with aging and aging related neurodegenerative disorders.
A committee of IOA and ADCC members will review all proposals. Funding depends on scientific merit, and the likelihood that the pilots will lead to independent funding to continue the research beyond the pilot studies. Priority will be given to:
• Faculty in the early stages of their career who seek to enter research fields on aging or AD and related neurodegenerative disorders
• Senior faculty who intend to shift their research emphasis towards aging or AD and related disorders
Application Process:
Applications will be considered for all pilot grant award programs, for which they are eligible, as described in this announcement, and they should be formatted in the style of a NIH PHS 398 application. However, a title page should be substituted for the NIH face page. Application items #5 and #6 below should be limited to 2 pages (exclusive of title page with abstract, budget, biosketches, other support, letters of collaboration, literature cited, etc. as in PHS 398). Animal and/or IRB protocols may be pending.
Organization of the application:
1) Title Page with Abstract (one page; not the NIH face page) showing the title of grant, name of PI, affiliation, address, telephone numbers and email address, as well as an abstract of the proposed project using language that an educated lay audience can understand
2) Budget (costs for personnel and supplies, but no tuition costs, equipment or instruments)
3) Biosketch
4) Other Support
5) Specific Aims
6) Research Strategy (Significance, Innovation, Approach)
7) Human Subjects (if applicable and protocol may be pending)
8) Vertebrate Animals Sections (if applicable and protocol may be pending)
9) Consultants (if applicable)
10) Consortium Contractual Arrangements (if applicable)
11) Literature Cited
12) Certification of Patient Oriented Research (if applicable)
It is obligatory that Pilot Awardees provide a final report at the end of the pilot year. Financial reports will also be required and Awardees must be responsive to subsequent requests for updates on publications and subsequent grants stemming from their Pilot as this information helps ensure the continuation of this program. In addition, IOA Pilot Awardees must present their pilot data at an IOA Retreat.
For more information, contact Kathryn Jedrziewski, IOA Deputy Director, at (215) 898-2445 or e-mail: jedrzmk@mail.med.upenn.edu.
Applications Due: February 6, 2015; anticipated date of award: July 1, 2015.
Submit one hardcopy original and an electronic PDF file (via email) to: Kathryn Jedrziewski, Institute on Aging, University of Pennsylvania, 3615 Chestnut Street, Philadelphia, PA 19104, jedrzmk@mail.med.upenn.edu.
Note: If anyone encounters difficulties with the email submission, please contact Kathryn Jedrziewski at the number listed above prior to the due date.
PA Dept of Aging Video Features PMC Caregivers
Are you one of the 15.5 million caregivers in the U.S.? This month we thank you as part of #NationalFamilyCaregiversMonth. The Pennsylvania Dept. of Aging also recognizes your commitment to helping others. Take a look at the video they produced featuring caregivers from the #PennMemoryCenter community.
Preclinical Detection of Alzheimer’s Disease Poses Some Unique Ethical Concerns
In the October 2014 issue of Medical Ethics Advisor, Jason Karlawish, MD, associate director of the Penn Memory Center, discusses the ethical concerns of preclinical detection of Alzheimer’s disease. “We operationalize our ethic of autonomy through our brain,” Dr. Karlawish says in the article.“So as we talk about labeling people’s brain at risk of decline before they are ill, we are playing with very hot ethical and social issues.”
You can read the article here.
University of Wisconsin Studies the Music and Memory Program
The University of Wisconsin-Milwaukee is leading a study on the impact of the Music and Memory Program, a music program aimed at helping dementia patients. Researchers are studying 1,500 Alzheimer’s and dementia patients who were given iPods at Wisconsin nursing homes through the program. They hope to determine whether music improves mood and behavior, which residents might benefit and then tailor activities accordingly. You can read more here.
Penn Joins the Nation’s Efforts to Promote Older Adults’ Brain Health
The University of Pennsylvania’s Prevention Research Center has been awarded two grants from the Centers for Disease Control (CDC) to advance the CDC’s Healthy Brain Initiative. Penn’s Prevention Research Center, directed by Karen Glanz, PhD, MPH, and Kevin Volpp, MD PhD, conducts innovative public health and disease research aimed at preventing chronic disease and reducing health disparities in Southeastern Pennsylvania. It is one of 26 CDC-supported Prevention Research Centers in the nation.
The “Healthy Brain Initiative Network Collaborating Center” will be led by Jason Karlawish, MD, associate director of the Penn Memory Center and director of the Alzheimer’s Disease Center’s Outreach, Recruitment and Education Core; and Amy Jordan, PhD, co-director of Penn PRC’s Communications and Dissemination Core. “Public Health Communications: Culturally Relevant Messages and Strategies to Promote Awareness about Dementia, including Alzheimer’s Disease” is a collaboration between Drs. Karlawish and Jordan to develop messages and a communication strategy to promote brain health and awareness about Alzheimer’s disease.
“We are thrilled that the CDC selected our proposals for funding,” said Dr. Karlawish. “The Healthy Brain Initiative is an important national effort to promote brain health for older Americans. These awards are a great opportunity for the Philadelphia region and Pennsylvania. They will connect the many smart, talented and motivated leaders in Philadelphia and Pennsylvania with a national effort to promote brain health.”
The goals of the Healthy Brain Initiative Network Collaborating Center are to participate in the Network’s efforts to establish and advance a research and service agenda in cognitive health and healthy brain aging, and support doctoral and postdoctoral education and training in cognitive health and healthy aging. The Center will develop a course “The public health implications of cognitive aging” for the masters in public health program, a certificate program in the Masters in Public Health program, and the “Healthy Brain Initiative Scholars,” for doctoral and post-doctoral students whose research focuses on cognitive health, cognitive impairment, Alzheimer’s disease or dementia.
The Center’s Advisory Board includes leaders in Alzheimer’s disease, aging, and research and health care services for older adults. The members include Brian Duke, Pennsylvania’s Secretary of Aging; Wendy Campbell, President and CEO of the Alzheimer’s Association’s Delaware Valley Chapter; Holly Lange, President and CEO of the Philadelphia Corporation for Aging; and Tinesha Banks, Deputy Executive Director of the Health Promotion Council.
“Public Health Communications: Culturally Relevant Messages and Strategies to Promote Awareness about Dementia, including Alzheimer’s Disease” is a collaboration between Dr. Karlawish and Dr. Jordan that will identify key issues related to communicating about cognitive health and Alzheimer’s disease. As part of this project, the investigators will design and develop public health messages focused on promoting cognitively healthy behaviors. Messages will be relevant for the two most common ethnic groups in the Philadelphia area, African Americans and non-Latino Whites.
Dr. Jordan, Associate Director of Policy Implementation for the Annenberg Public Policy Center at the University of Pennsylvania, has a wealth of experience developing and disseminating public health messages. She explains that “effective messaging to promote healthy behaviors must be done with a solid framework of evidence that supports the targeted behavior and the messages people see. With the support of the CDC, we will be part of a national effort to begin this for brain health. This is a great opportunity to have a national impact.”
These grants are part of the CDC’s Healthy Brain Initiative, inaugurated in 2005, that addresses the public health challenges of cognitive aging and Alzheimer’s disease. The goals of the Initiative’s Road Map for State and National Partnerships, 2013-2018 include developing and disseminating culturally relevant public health messaging about brain health and Alzheimer’s disease.
A total of $12.3 million was awarded to 21 Prevention Research Centers for 56 Special Interest Projects to design, test, and disseminate effective applied public health prevention research strategies. The UPenn Prevention Research Center received 4 awards. To view a complete list of the 2014 awards, click here.
PMC Choral Group in the News
Darina Petrovsky, a predoctoral student at the University of Pennsylvania School of Nursing, and the leader of the Penn Memory Center Choral Group, spoke to WRTI Radio (90.1 FM) about the benefits of singing as a group, including developing new friendships and reducing stress.
You can listen to her interview here, and also hear clips from the group’s performance in May at the Watermark at Logan Square.
Do you know someone who is interested in joining the group? Our fall session is just beginning. Please contact barbara.overholser@uphs.upenn.edu for more information.
Too Young to Die, Too Old to Worry
Two years ago, at a conference in Miami on Alzheimer’s disease, after a session about risk factors and biomarker prediction models, a colleague remarked to Jason Karlawish, M.D., how the singer Leonard Cohen has been saying onstage that when he turns 80, he will resume smoking. As he pondered that comment, Alzheimer’s biomarkers and our zeal to foresee our future, Dr. Karlawish began to think of an essay to take on the question, “When should we set aside a life lived for the future and, instead, embrace the pleasures of the present?”
The essay was published last week in the New York Times, and you can read it here.
Madness and Memory: The Discovery of Prions—A New Biological Principle of Disease
In the current issue of The Pennsylvania Gazette you’ll find Penn Memory Center‘s Dr. Jason Karlawish’s review of Nobel Prize winning researcher Stanley Prusiner’s memoir, “Madness and Memory: The Discovery of Prions—A New Biological Principle of Disease.” The memior traces Prusiner’s journey from his Midwestern boyhood to his 1997 Nobel Prize in Physiology/Medicine for his work determining prions as among the causes of neurological diseases.. Prusiner is now director of the Institute for Neurodegenerative Diseases and professor of neurology at the University of California, San Francisco.
In the review, Dr. Karlawish asks, “In the life of the scientist, is there life outside of science?”
You can read the review here.
Medicare to Start Paying Doctors Who Coordinate Needs of Chronically Ill Patients
Starting in 2015, Medicare will pay monthly fees to doctors who manage care for patients with two or more chronic conditions. This is a policy change initiated by the Obama administration.
In an interview in the New York Times, Marilyn B. Tavenner, the administrator of the Centers for Medicare and Medicaid Services said, “Paying separately for chronic care management services is a significant policy change.” The article noted that care coordination could pay for itself by keeping patients healthier and out of hospitals.
“This is great news for our patients at the Penn Memory Center,” says Jason Karlawish, MD, Associate Director of the Penn Memory Center.
“Persons with Alzheimer’s disease and other cognitive disorders typically have other common medical illnesses as well. Taking care of them requires organizing and coordinating information, and communication among disciplines and the patient’s family. It’s a rewarding part of practicing medicine but it’s time intensive.”
You can read the New York Times article here.
Absence of Gene May Help Fight Alzheimer’s
A study published in JAMA Neurology on August 11, 2014, suggests that minimizing apoE gene levels in the brain may be an approach to developing a treatment for Alzheimer’s disease. In the study, researchers found that a man with no apolipoprotein E, or apoE, in his body was cognitively normal and showed no neurological signs of Alzheimer’s. Those with a mutation of the gene called apoE4 have a higher risk of developing Alzheimer’s. You can read the study here.
ARTZ Philadelphia
The Philadelphia Inquirer reported on ARTZ Philadelphia’s programming for people with dementia, and the organization’s relationship with the Penn Memory Center. The organization’s goal is to serve, through arts and culture, people with Alzheimer’s and other forms of dementia. The Penn Memory Center is working closely with the organization to spread the word about its museum tours and arts activities. You can read the Philadelphia Inquirer article here.
Testing a New Approach to Alzheimer’s
Alzheimer’s disease experts are testing an unusual approach to the disease: giving the brain what may be a more efficient source of energy. In people with Alzheimer’s and other dementias, the brain loses its ability to properly metabolize glucose early in the course of disease. Several sites are now testing AC-1204, a vanilla-flavored white powder that supplies a type of triglycerides. Steven Arnold, MD, director of the Penn Memory Center, said he was skeptical of the “alternative energy” argument. “Why dying cells can use this energy source better than glucose has never been clear to me,” he told the Philadelphia Inquirer.
You can read the Philadelphia Inquirer article here.
Lifestyle Changes May be Important in Reducing Alzheimer’s Risk
USA Today, citing a Finnish study presented on Sunday, July 13, 2014 at the Alzheimer’s Association International Conference in Denmark, says that everyday health activities can reduce someone’s risk of memory decline. The study is the first to examine the impact of the combination of eating well, exercising, keeping mentally and socially engaged, and managing obesity, high blood pressure and diabetes; other studies have looked at pieces of healthy lifestyles, but not the combination.
You can read the USA Today article here.
Is the USPSTF Right About Early Screening For Cognitive Impairment?
An article in the June 2014 issue of Managed Care examines the U.S. Preventive Services Task Force’s recent recommendation declaring that there is currently insufficient evidence to recommend early cognitive screening.
Author Susan Worley interviewed a number of experts in the field of Alzheimer’s disease treatment and research including Jason Karlawish, MD, professor of medicine, medical ethics, and health policy at the University of Pennsylvania, and Associate Director of the Penn Memory Center.
“Cognitive screening in a general population is obviously wrong,” says Dr. Karlawish. “Screening really must be focused on an older population. The lower we set the age, the more we increase the chance of false positive detection. I’m in favor of screening when the probability that you are going to pick up cognitive impairment is reasonably high, and that is in the setting of practices that care for older adults. Among geriatricians, I would say, it is a fairly standard practice to assess your patients’ cognition.”
You can read the article here.
Elderly Shown to Need Theft Safeguards
American seniors have lost an estimated $2.9 billion in financial scams in the last decade, and financial institutions need to do more to protect them, experts suggested at a meeting on Monday. June 16.
Jason Karlawish, MD, professor of Medicine and Medical Ethics and Health Policy, told the Philadelphia Inquirer that this is a public health problem and called for a “reboot” of the financial services industry.
“Who are these people selling stuff to seniors as their job?” he asked at a panel on financial abuse of the elderly, sponsored by the United Way in Center City. Though he hates the terms, he said, such people should become “senior certified” or “senior friendly.”
You can read the Philadelphia Inquirer article here.
Meet the First Two Penn Memory Center A4 Trial Participants
Myrna Roach and Donald Jackson are the Penn Memory Center’s first two participants in the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s study (the “A4 study”), a historic prevention trial which is testing whether a new investigational treatment, called an amyloid antibody, can slow memory loss caused by Alzheimer’s disease.
“There’s a family history of Alzheimer’s disease,” says Ms. Roach, “so I’m interested in helping to find a cure for it, maybe in my lifetime.”
For more information about the A4 trial, click here.
A4 Trial Begins; First Patient Receives Infusion in Providence, RI
The A4 study is underway to see if an experimental drug can protect healthy seniors whose brains harbor silent signs that they’re at risk. On June 9, a Rhode Island man was hooked up for an IV infusion at Butler Hospital in Providence, the first treated. The $140 million study, funded by the National Institutes of Health, Eli Lilly & Co., and others, will track if participants’ memory and amyloid levels change over three years. The study is enrolling participants at more than 60 sites, including the Penn Memory Center. In an AP article published in June, Dr. Jason Karlawish, Associate Director of the Penn Memory Center, and a designer of the study’s psychological precautions, calls the research “an opportunity to study the future of the way we’re going to think about, talk about and live with the risks of Alzheimer’s disease.” You can read the AP article here.
Is There a Disease in Your Future?
In a Portland Tribune (Ore.) article about predictive tests for neurodegenerative diseases, Jason Karlawish, MD, professor of Geriatrics and Medical Ethics and Health Policy, says most physicians don’t want to be bothered with predictive tests. Karlawish directs the Neurodegenerative Disease Ethics and Policy Program at the Penn Memory Center. Karlawish says even the most predictive tests such as a genetic test for Huntington’s are inexact. They don’t tell those who test positive when they will get the disease. One study of people learning they tested positive for a gene associated with Alzheimer’s, according to Karlawish, did not show significant numbers of them lapsing into long-term depression or becoming markedly anxious.
You can read the article here.
IOA and ADCC Award Grants
The University of Pennsylvania Institute on Aging (IOA) and Alzheimer’s Disease Core Center (ADCC) awarded two one-year pilot grants focusing on Alzheimer’s disease (AD) and related neurodegenerative disorders.
“Does Chronic Insomnia Lead to Accumulation of Beta Amyloid?” Philip Gehrman, PhD’s pilot study, will measure beta amyloid and other metabolites in five individuals with chronic insomnia and compare them to five good sleepers. Dr. Gehrman, Assistant Professor in the Department of Psychiatry at the Perelman School of Medicine, University of Pennsylvania, says that the results of the study may help investigators understand how chronic poor sleep may increase the risk for dementia, and inform the development of interventions designed to reduce the likelihood of dementia.
David R. Roalf, PhD, a Research Associate at the the University of Pennsylvania Perelman School of Medicine, Department of Psychiatry, will be focusing on early indicators and detection of cognitive impairments. His pilot study, “Within-individual Variability as a Biomarker of Incipient Dementia in Mild Cognitive Impairment,” will measure neurocognitive variability in individuals with Alzheimer’s disease, Mild Cognitive Impairment and healthy aging to better understand the utility of the fluctuations in neurocognitive ability as an indicator of neurological integrity and its viability as an early indicator of cognitive impairment in MCI.
Poll Says it is More Stressful Caring for Spouse Than Parent
An Associated Press – NORC Center for Public Affairs Research poll of Americans shows becoming a caregiver to a frail spouse causes more stress than having to care for a parent or an in-law.
While 8 in 10 people who’ve been caregivers called it a positive experience, it’s also incredibly difficult. And while 7 in 10 who cared for a spouse said their relationship grew stronger as a result, nearly two-thirds said it caused stress in their family compared with about half among those who cared for a parent.
You can read more about the poll here.
Penn Memory Center Choral Group Performance at the Watermark
The Penn Memory Center Choral Group, led by Darina Petrovsky, a Penn Nursing Science PhD student, gave a fantastic performance at The Watermark at Logan Square. Over the course of 4 months, the group rehearsed a selection of Eastern Orthodox Easter music, Russian folk songs and American favorites. The performance closed with a rousing sing-along of America the Beautiful. Click here to see photos.
Home Safety for People with Alzheimer’s Disease
Caring for a person with Alzheimer’s disease, and keeping them safe, can be challenging. The National Institutes of Health (NIH)‘s ADEAR center offers a booklet for caregivers with suggestions for creating a safer space for people with Alzheimer’s disease.
Step 1? Think prevention.
You can download the booklet here.
AARP Bulletin Reports on Reaction to a Potential Blood Test for Alzheimer’s Disease
The AARP Bulletin reports on reaction to a potential blood test for Alzheimer’s disease. While some experts heralded the news, others worried that, until effective treatments are available, learning that you’re likely to develop Alzheimer’s could cause more harm than good. There’s already good evidence that simple lifestyle changes can help slow the likelihood of developing dementia, says Jason Karlawish, MD, professor of Medicine and Medical Ethics and Health Policy, and Associate Director of the Penn Memory Center, who was not involved in developing the test. “A heart-healthy diet, physical activity, and social and cognitive stimulation can help preserve cognitive function,” he says. People who learn that they are at high risk of developing Alzheimer’s may be more motivated to make healthy changes.
Click here to read more.
Taking Care of the Caregiver
Taking care of yourself is one of the most important things you can do as a caregiver. Regular physical activity can help you increase your energy levels needed for caregiving activities, prevent chronic diseases, and reduce feelings of depression or stress.
Worried about finding the time to exercise? Make a plan to exercise with the person you care for because people with Alzheimer’s disease can benefit from exercise, too.
Here are some ideas to help get you going: Exercise and Physical Activity: Alzheimer’s Caregiving Tips.
The Long Reach of Alzheimer’s Disease
The April issue of the journal Health Affairs is devoted to “the long reach of Alzheimer’s disease.” The issue examines research, national policy, caregiver support, and end-of-life care in an expansive collection of 28 articles.
A large portion of the journal issue concentrates on supporting people with the disease. “Our role is to make the case for caregivers and patients currently in need,” said Sarah Dine, senior deputy editor of Health Affairs. She hopes the journal will increase awareness about their plight and inspire good policy. “It’s hard to get funding for care managers who are training for the workforce, or support for family caregivers on the ground,” she told Alzforum.org.
One urgent problem is that people caring for Alzheimer’s patients have few options for guidance or help. “The healthcare system largely neglects caregiving,” said Jason Karlawish, Associate Director of the Penn Memory Center.
“Although multiple randomized controlled trials have shown that education, skill training, and support benefit not just the caregiver, but the patient, we don’t provide those interventions as a matter of routine care,” he said. “That simply has to change.”
Read more at Alzforum. org
We All Have Alzheimer’s
Jason Karlawish, MD, professor of Medicine, Medical Ethics and Health Policy, speaks with WTOP radio in Washington, D.C. about his Health Affairs paper looking at ways society can prepare for living with Alzheimer’s disease. “If you have a patient with dementia, you invariably have at least one other person who has to take care of that person,” said Karlawish.
“They start to have Alzheimer’s disease…they live the disease, they think about the disease, they make decisions for the patient, so in some sense, the disease is as much their own experience as it is, of course, for the patient. Now is the time to be thinking about living with a brain at risk.”
“Whether as patients or as caregivers, we all have Alzheimer’s disease,” says Karlawish. “The question we must engage with is, How should we live with it?”
You can read more here. Listen to the interview with Dr. Karlawish on WTOP Radio here.
