By Alison Lynn, Penn Memory Center Director of Social Work
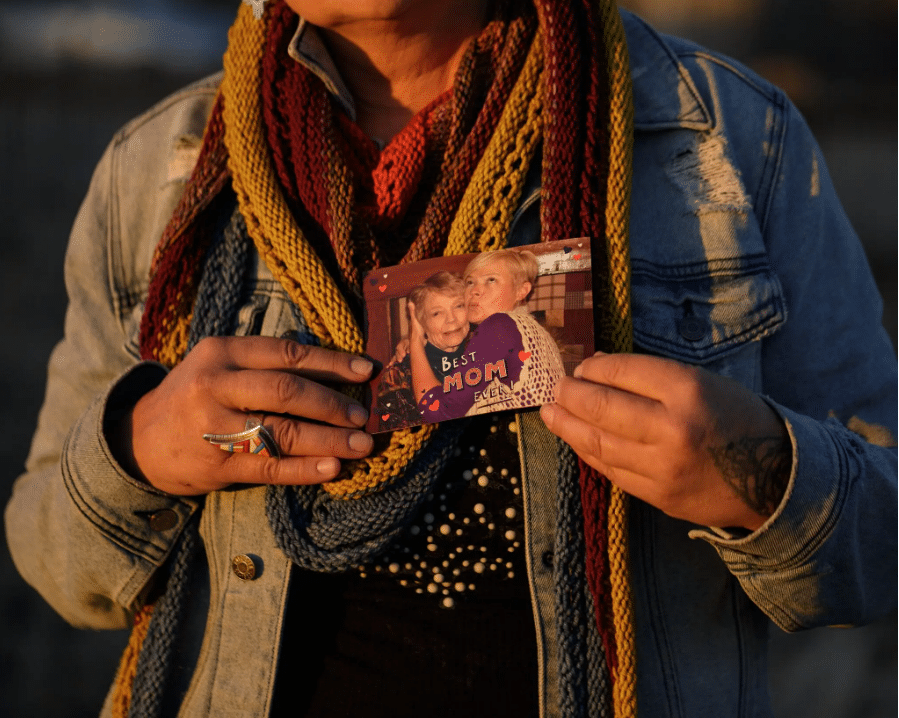
Diane’s daughter holding a picture of her and her mother. Credit: McNair Evans for The New York Times
A Story of Dementia: The Mother Who Changed
Katie Engelhart (whose book, “The Inevitable: Dispatches on the Right to Die,” I also highly recommend) explores the complexities of selfhood, decision-making capacity, and caregiving in her heartbreaking story on the Norelius family.
Engelhart traces the story of Diane Norelius, whose diagnosis of dementia led to a years-long financial and legal conflict between her daughters and her new romantic partner. Diane’s personality changed, which led her to start a relationship with a man who her daughters allege was financially manipulating her and neglecting her care. Her partner, of course, accused her daughters of the same thing.
Through this family saga, Engelhart illuminates a core ethical dilemma in dementia care: whose wishes should caregivers seek to honor — those of ‘pre-diagnosis Diane,’ or those of the Diane standing in front of them? And what if those presentations of self and wishes fluctuate? There’s not one right answer here, and Engelhart avoids any kind of pat conclusion to the story.
Even though I’ve heard versions of this story over and over again in my work, I was riveted by this well-reported piece. What’s newsworthy is that this isn’t an anomaly — it happens all the time.
Matt Chase / The Atlantic. Sources: Getty; Unsplash.
How People with Dementia Make Sense of the World
Dasha Kiper’s piece for The Atlantic is an excerpt from her illuminating book “Travelers to Unimaginable Lands: Stories of Dementia, Caregivers and the Human Brain.” With great compassion, Kiper uses stories from her time providing therapy to dementia caregivers to illustrate how the workings of a healthy brain makes it difficult for us to understand and meet the needs of those whose brain is sick.
A common refrain among caregivers in our clinic is “I understand intellectually why my spouse is asking me the same question over and over again, but I am still struggling to adjust my emotional response.” Or, “Even though I know my parent is not purposefully ignoring or manipulating me, it certainly seems that way. After all, they can act like nothing is wrong in public!” Caregivers often say this with a sense of shame, as if they should be able to easily overcome one of the toughest and most confusing experiences a person can go through. While Kiper does provide the same reassurance that I would, she takes it a step further by exploring the mechanisms of our minds that make it so difficult to do just that. In other words, it’s not your fault that you can’t always “just accept” that the person in front of you is different than they have been — your brain isn’t hardwired or socialized to understand it.
Dementia Care Tips from Adria Thompson
Adria Thompson is a speech-language pathologist who posts short videos to help family caregivers improve their understanding of dementia, and to improve their caregiving skills.
If you as a caregiver are overwhelmed by the sheer number of “how to” books available to you and prefer smaller chunks of information, I cannot recommend this page highly enough.
Adria’s account is a mix of disease education (“What is the FAST scale?”), suggestions for managing common behavioral symptoms of dementia (“theft accusations”), tutorials for common issues in hands-on caregiving (“How to move someone with paratonia”), and encouragement for caregivers (“When someone goes to a long-term care community, it is not a sign of failure”). Even the comments sections on her posts provide a wealth of support and community from other caregivers around the world.