By Christine Willinger
Over the past 25 years, biomedical research has revolutionized the diagnosis of Alzheimer’s disease (AD). Once based solely on clinical signs and symptoms, today’s diagnosis involves advanced methods that can detect neurodegeneration far earlier than before, including imaging and biological fluids.
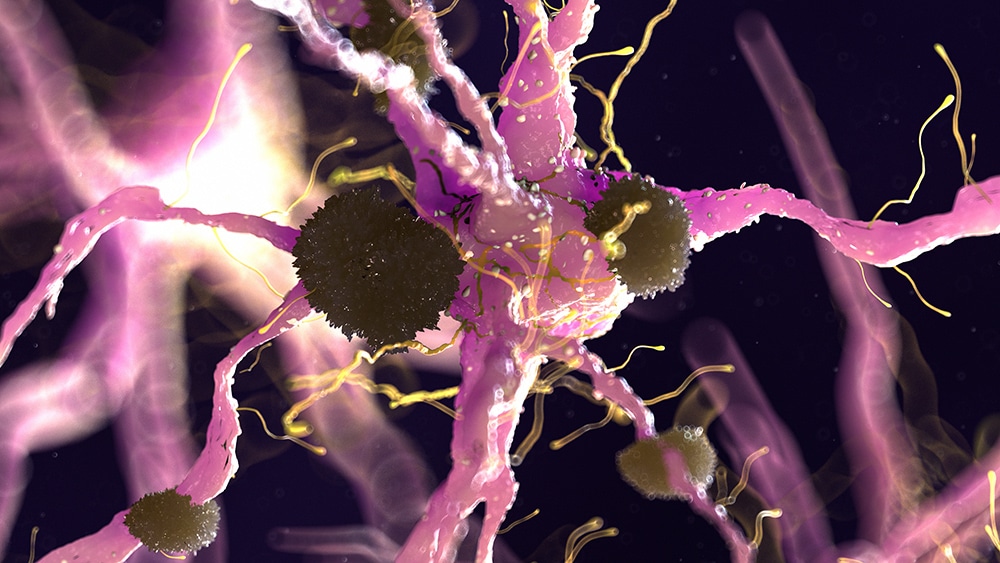
The National Institution On Aging and the Alzheimer’s Association recently released an updated research framework that proposes a new biomarker-based paradigm for the diagnosis of AD. This research framework is described as the AT(N) system: A stands for B-amyloid plaques, T for tau neurofibrillary tangles, and N for neurodegeneration.
Amyloid and tau can be measured by positron emission tomography (PET) imaging or in cerebrospinal fluid (CSF), while neurodegeneration can be evaluated by magnetic resonance imaging (MRI) or PET. Patients can then be categorized based on the presence or absence of each biomarker into eight separate diagnostic groups–for example, A+T-(N+).
Importantly, this research framework must be rigorously tested in real patients to determine its usefulness for clinical care. Earlier this month, researchers at the Mayo clinic published an article in the Journal of the American Medical Association that began to do just that.
The researchers measured B-amyloid and tau using PET and neurodegeneration using MRI in older adults without dementia at baseline. They found that participants’ AT(N) group, when added to traditional clinical and genetic factors, increased the researchers’ ability to predict participants’ rate of memory decline over the next five years.
Although the predictive power of the AT(N) system was relatively small, AT(N) groups with a greater number of positive biomarkers experienced significantly higher rates of memory decline, equivalent to being 20 years older at baseline. As David Wolk, Co-Director of Penn Memory Center and author of an accompanying editorial, explained, these data suggest a “potentially useful role of AD biomarkers in forecasting clinical course.”
These findings could also have direct relevance for patients involved in AD clinical trials. Dr. Wolk noted that the AT(N) system may allow “patients to be categorized into distinct prognostic groups that are more or less informative regarding therapeutic agent effects.” In other words, this system might enable researchers to better target treatments in clinical trials to the participants most likely to benefit from them, based on their biology.
Dr. Wolk also pointed out several limitations to this work. It is unclear whether and to what extent AD biomarker measurements should be adjusted for age, and AT(N) neuroimaging will be prohibitively expensive in many settings. Nevertheless, he was encouraged by “this important contribution […] to advancing the conceptualization of AD.”