Eli Lilly and Company announced this week that solanezumab did not slow the progression of cognitive decline due to Alzheimer’s disease (AD) pathology when initiated in individuals with amyloid plaque but no clinical symptoms of the disease, known as the preclinical stage of AD.
Solanezumab only targets soluble amyloid beta. The treatment did not clear plaque or halt accumulation of amyloid in participants treated with the drug in the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s disease (A4) Study.
“Results of the A4 Study clearly showed that the primary and secondary endpoints were not met. Therefore, the A4 Study concludes our clinical development of solanezumab and indicates that targeting soluble amyloid beta through this mechanism is not effective in this population,” said John Sims, head of medical, global brand development – solanezumab, for Eli Lilly and Company. “While this study was negative, the unique data generated have increased our understanding of preclinical Alzheimer’s disease and will advance the next generation of AD prevention studies. Raw data and analyses will be made widely available to researchers through the public-private partnership with the NIH-funded Alzheimer’s Clinical Trial Consortium. These data will serve the scientific community and enable Lilly and other drug developers to enhance our clinical trial designs for other potential medicines targeting Alzheimer’s disease.”
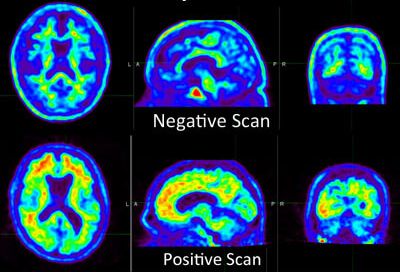
Launched in 2013, the A4 Study was a first-of-its-kind secondary prevention trial, enrolling more than 1,100 individuals between 65 and 85 years of age who had PET-imaging evidence of amyloid plaque accumulation in the brain and who did not have clinical impairment. Participants were randomized to either solanezumab or placebo and then treated for approximately 4.5 years.

Sanjeev Vaishnavi, MD, PhD
“This is a disappointing result for the research community but particularly for the study volunteers and their study partners who have supported the project for the last decade,” said Sanjeev Vaishnavi, MD, PhD, who oversaw the A4 study at the University of Pennsylvania. “We are so grateful to have had a dedicated cohort throughout the study, and we’ll continue to make the most out of all of our available data, even after the study’s conclusion.”
Solanezumab binds only to soluble amyloid-beta protein and was not expected to significantly remove deposited amyloid plaques. Donanemab and remternetug, other Lilly investigational antibodies currently being developed in Phase 3, are different from solanezumab in that they specifically target deposited amyloid plaque and have been shown to lead to plaque clearance in treated patients.
More than 6.5 million Americans are currently suffering from dementia due to Alzheimer’s disease, and scientists expect this number to nearly triple by 2050. It is estimated that more than 20 million Americans and approximately 315 million people globally have preclinical Alzheimer’s disease, the earliest stages of the disease.
During the double-blind portion of the study, results showed:
- Solanezumab did not slow cognitive decline on the primary outcome measure, the Preclinical Alzheimer Cognitive Composite (PACC) [mean change (95% CI): placebo -1.4 (‑1.76, ‑1.04); solanezumab -1.69 (-2.13, -1.26); p-value 0.26)]. The PACC was developed to measure the aspects of cognitive decline relevant in preclinical AD and is an equally weighted composite that tests episodic memory, timed executive function, and global cognition.
- Secondary clinical outcome results were consistent with the primary outcome, numerically favoring placebo compared with solanezumab.
- 36.1% of participants starting at the stage of preclinical AD progressed on the Clinical Dementia Rating-Global Scale (defined as CDR-global score greater than 0 at two consecutive visits or final visit). CDR-GS is a clinician-rated scale that provides an overall assessment of the participant’s clinical stage of AD. Similar rates of progression were seen with both the solanezumab and placebo groups.
- On amyloid PET imaging, amyloid continued to accumulate over time in both the placebo (65.9 Centiloid baseline, 17.5 Centiloid increase) and solanezumab (66.2 Centiloid baseline, 12.1 Centiloid increase) groups.
- Higher baseline amyloid levels were strongly associated with a greater risk of progression to symptomatic Alzheimer’s disease (p-value<0.001).
- The solanezumab and placebo groups were well-balanced at baseline, and results were consistent across multiple analysis methods and models.
- Safety results in the A4 Study were consistent with the safety profile observed in previous solanezumab Phase 3 studies. Amyloid-Related Imaging Abnormalities with edema/effusion (ARIA-E) were uncommon and similar between treatment and placebo groups.
“These findings indicate that amyloid is a key driver of cognitive decline at the preclinical stage of Alzheimer’s disease. Solanezumab did not substantially impact amyloid plaque burden in the brain, and unfortunately did not slow cognitive decline. These data suggest that we may need to be more aggressive with amyloid removal even at this very early stage of disease,” said Reisa Sperling, M.D., a neurologist at the Brigham and Women’s Hospital, Harvard Medical School and the A4 Study project director. “We are so very grateful to the participants, their study partners, the clinical trial site investigators and staff, and the entire study team for their longstanding dedication to this important study. It is imperative that we learn everything we can to inform ongoing and future trials in our quest to prevent memory loss due to Alzheimer’s disease.”
The A4 Study is a landmark public-private partnership, funded by the National Institute on Aging (part of National Institutes of Health), Eli Lilly and Company, Alzheimer’s Association, GHR Foundation, Foundation for the National Institutes of Health, and several other organizations and donors. The A4 Study is coordinated by the Alzheimer’s Therapeutic Research Institute (ATRI) at the Keck School of Medicine of University of Southern California and is a project of the Alzheimer’s Clinical Trials Consortium (ACTC).
Full disclosure of the study results will be shared later in the year at a scientific conference.